UnitedHealthcare has announced their 2023 ACA new member and retention bonus program. This bonus will apply to all new sales and renewals of UnitedHealthcare Individual and Family Exchange plans that are effective in 2023. Take a look at how much you can earn!
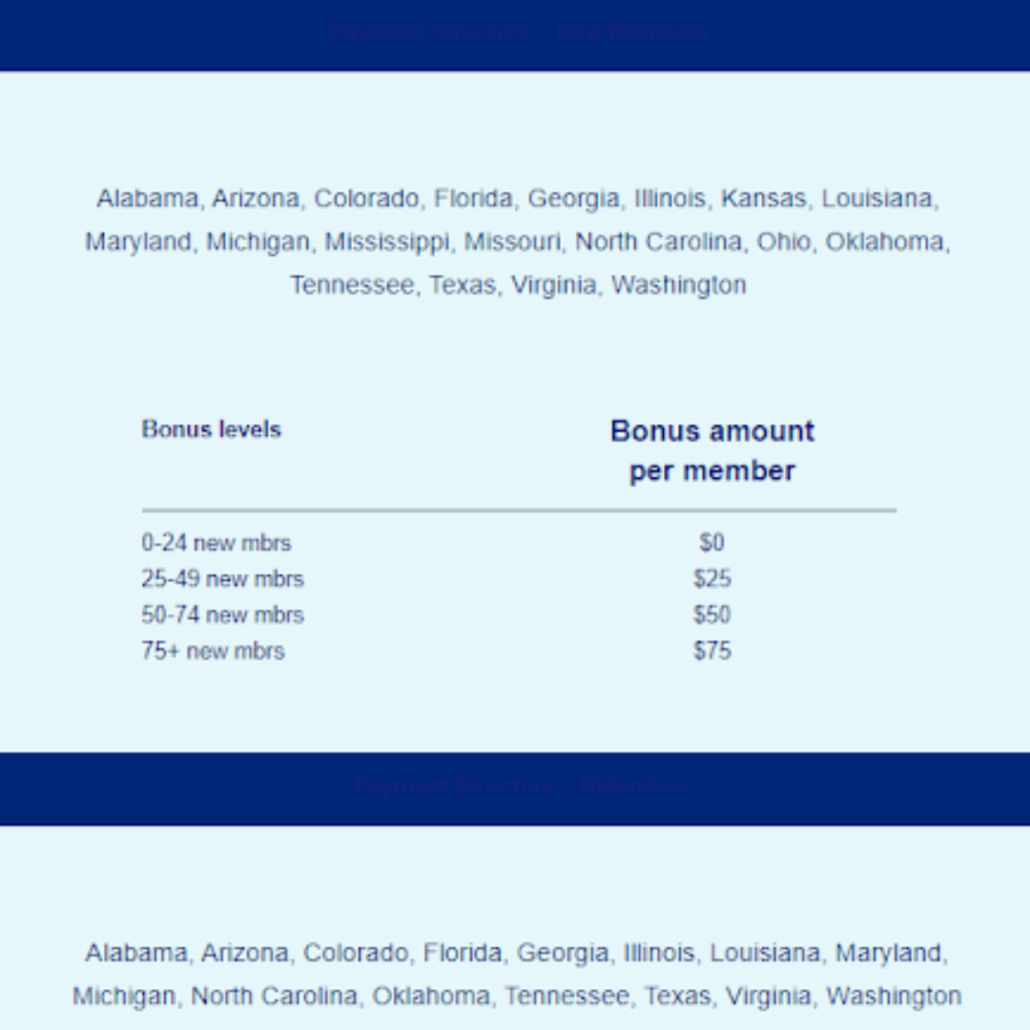
- Bonus Program applies to sales of UnitedHealthcare Individual and Family Plans in AL, AZ, CO, FL, GA, IL, KS, LA, MD, MI, MO, MS, NC, OH, OK, TN, TX, VA, WA with Jan. 1, 2023, through Dec. 1, 2023, effective dates
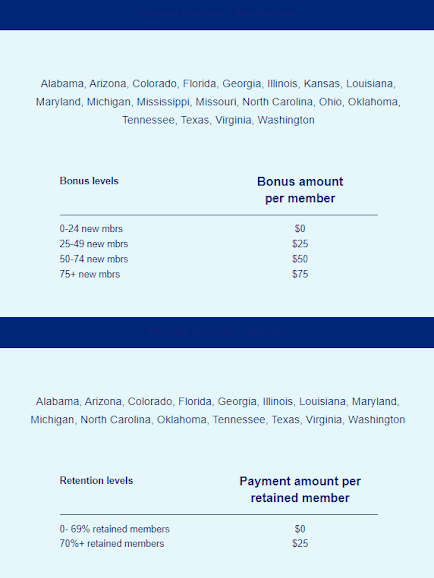
- Retention Program applies to membership enrolled in a UnitedHealthcare Individual and Family Plan in AL, AZ, CO, FL, GA, IL, LA, MD, MI, NC, OK, TN, TX, VA, WA as of Dec. 31, 2022, who remain enrolled through March 1, 2023
- All payment amounts listed above are a one-time bonus payment per effectuated member in the program year
- All Bonus Program payments will be calculated each quarter by the total number of UnitedHealthcare Individual and Family Plan effectuated members within each state. New business qualification levels will reset at the end of each quarter
- Retention Program payments will be made no later than March 31, 2023
- For effectuated members with applications received on or before March 31, 2023, Bonus Program Payments will be made no later than June 29, 2023 (Q1 payment)
- For effectuated members with applications received between April 1, 2023, and before June 30, 2023, Bonus Program Payments will be made no later than Sept. 28, 2023 (Q2 payment)
- For effectuated members with applications received between July 1, 2023, and before Sept. 30, 2023, Bonus Program Payments will be made no later than Dec. 29, 2023 (Q3 payment)
- For effectuated members with applications received between Oct. 1, 2023, and before Dec. 31, 2023, Bonus Program Payments will be made no later than March 29, 2024 (Q4 payment)
- There is no cap on the Bonus Program or Retention Program
- All eligible UnitedHealthcare Individual and Family Plans must be in force for a minimum of 3 months from the effective date to count as “issued.” Coverage must be in force with premium payment current at the time of contest payout to be included. If coverage is terminated for any reason prior to 3 months, the broker will be charged back for any difference if it alters the bonus amount paid
- Applies to both On- and Off-Exchange business
- If a broker assigns commissions to an agency, the bonus payment will be paid to the agency rather than the individual broker following our standard commission payout practices
- Broker must meet all compliance requirements and be appointed by the applicable UnitedHealthcare carrier in the state of this program