
Dual eligible special needs plans (DSNP) are a type of Medicare and Medicaid coverage that are tailored to meet the specific needs of certain individuals. DSNPs provides access to a wide range of services and benefits designed to help individuals with long-term care needs and help them maintain their independence in the home or in a care setting. DSNPs cover all Medicare-covered services, plus additional services and benefits, and are available for individuals who are eligible for both Medicare and Medicaid. With DSNPs, individuals can obtain the coordinated care, services, and supports that are best suited to their needs, and access quality care at a lower cost.
Knowing the difference between Aetna Medicare and Medicaid dual plans
Aetna Medicare and Medicaid dual plans provide a comprehensive healthcare solution for those who are eligible for both Medicare and Medicaid. These plans combine the benefits of both programs and often include additional benefits such as dental, vision, and prescription drug coverage. The plans also typically come with low copayments, coinsurance, and no annual deductible. However, it is important to note that these plans do not cover services and treatments that are not covered by either Medicare or Medicaid. Furthermore, Medicare and Medicaid dual plans are usually more expensive than plans offered by other private health insurers, as they require two separate premiums.
Which of your customers are eligible for dual eligible special needs plans?
Individuals who are entitled to both Medicare (title XVIII) and medical assistance from a state plan under Medicaid (Title XIX) are eligible for Dual Eligible Special Needs Plans. These plans offer many benefits, including a $0 monthly premium, a $0 Rx copay, and coverage for some Medicare costs depending on the individual’s state and eligibility. To be eligible for a Dual Eligible Special Needs Plan, individuals must qualify for Medicaid and/or receive financial help, have Medicare Parts A and B, and live in the plan’s service coverage area.
What your customers should know about Aetna D-SNP
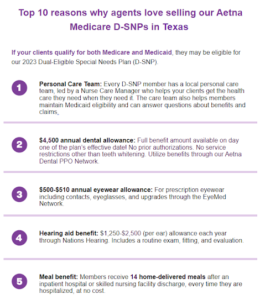
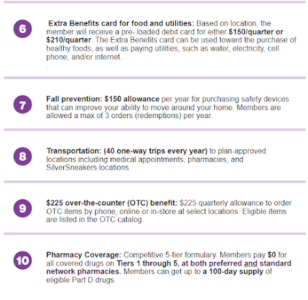
Aetna Dual Eligible Special Needs Plans (D-SNP) are designed to provide tailored care and coverage for those who are eligible for both Medicare and Medicaid. These plans provide an array of additional benefits and services not covered under traditional Medicare, such as dental, hearing aids, contact lenses, and more. It is important to note that in order to remain a member of these plans, you must continue to reside in the plan service area. Additionally, be aware of any suspicious calls, texts, or emails about “free” coronavirus testing and report any scams to the appropriate authorities.
What your customers need to know about Dual Eligible Special Needs Plans in Texas
These plans offer Medicare zero-dollar cost sharing and are available in six Texas counties: Bexar, Dallas, El Paso, Harris, Hidalgo, and Tarrant. Individuals may be eligible for D-SNPs if they have a chronic condition, are living in an institution, or fail to qualify for other Medicare Advantage plans. D-SNPs also offer additional benefits not found in Original Medicare, such as vision, dental, and prescription drug coverage.
Are you contracted to sell Aetna Medicare yet? Learn why thousands of health insurance agents love being a part of the Agility family!




